Jeong+Ho+Lee
-
 A Mechanism Underlying Most Common Cause of Epileptic Seizures Revealed
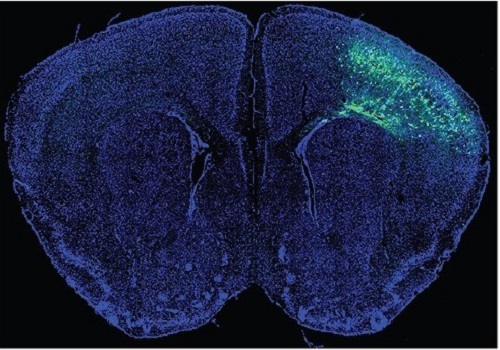
An interdisciplinary study shows that neurons carrying somatic mutations in MTOR can lead to focal epileptogenesis via non-cell-autonomous hyperexcitability of nearby nonmutated neurons
During fetal development, cells should migrate to the outer edge of the brain to form critical connections for information transfer and regulation in the body. When even a few cells fail to move to the correct location, the neurons become disorganized and this results in focal cortical dysplasia. This condition is the most common cause of seizures that cannot be controlled with medication in children and the second most common cause in adults.
Now, an interdisciplinary team studying neurogenetics, neural networks, and neurophysiology at KAIST has revealed how dysfunctions in even a small percentage of cells can cause disorder across the entire brain. They published their results on June 28 in Annals of Neurology.
The work builds on a previous finding, also by a KAIST scientists, who found that focal cortical dysplasia was caused by mutations in the cells involved in mTOR, a pathway that regulates signaling between neurons in the brain.
“Only 1 to 2% of neurons carrying mutations in the mTOR signaling pathway that regulates cell signaling in the brain have been found to include seizures in animal models of focal cortical dysplasia,” said Professor Jong-Woo Sohn from the Department of Biological Sciences. “The main challenge of this study was to explain how nearby non-mutated neurons are hyperexcitable.”
Initially, the researchers hypothesized that the mutated cells affected the number of excitatory and inhibitory synapses in all neurons, mutated or not. These neural gates can trigger or halt activity, respectively, in other neurons. Seizures are a result of extreme activity, called hyperexcitability. If the mutated cells upend the balance and result in more excitatory cells, the researchers thought, it made sense that the cells would be more susceptible to hyperexcitability and, as a result, seizures.
“Contrary to our expectations, the synaptic input balance was not changed in either the mutated or non-mutated neurons,” said Professor Jeong Ho Lee from the Graduate School of Medical Science and Engineering. “We turned our attention to a protein overproduced by mutated neurons.”
The protein is adenosine kinase, which lowers the concentration of adenosine. This naturally occurring compound is an anticonvulsant and works to relax vessels. In mice engineered to have focal cortical dysplasia, the researchers injected adenosine to replace the levels lowered by the protein. It worked and the neurons became less excitable.
“We demonstrated that augmentation of adenosine signaling could attenuate the excitability of non-mutated neurons,” said Professor Se-Bum Paik from the Department of Bio and Brain Engineering.
The effect on the non-mutated neurons was the surprising part, according to Paik. “The seizure-triggering hyperexcitability originated not in the mutation-carrying neurons, but instead in the nearby non-mutated neurons,” he said.
The mutated neurons excreted more adenosine kinase, reducing the adenosine levels in the local environment of all the cells. With less adenosine, the non-mutated neurons became hyperexcitable, leading to seizures.
“While we need further investigate into the relationship between the concentration of adenosine and the increased excitation of nearby neurons, our results support the medical use of drugs to activate adenosine signaling as a possible treatment pathway for focal cortical dysplasia,” Professor Lee said.
The Suh Kyungbae Foundation, the Korea Health Technology Research and Development Project, the Ministry of Health & Welfare, and the National Research Foundation in Korea funded this work.
-Publication:Koh, H.Y., Jang, J., Ju, S.H., Kim, R., Cho, G.-B., Kim, D.S., Sohn, J.-W., Paik, S.-B. and Lee, J.H. (2021), ‘Non–Cell Autonomous Epileptogenesis in Focal Cortical Dysplasia’ Annals of Neurology, 90: 285 299. (https://doi.org/10.1002/ana.26149)
-ProfileProfessor Jeong Ho Lee Translational Neurogenetics Labhttps://tnl.kaist.ac.kr/ Graduate School of Medical Science and Engineering KAIST
Professor Se-Bum Paik Visual System and Neural Network Laboratory http://vs.kaist.ac.kr/ Department of Bio and Brain EngineeringKAIST
Professor Jong-Woo Sohn Laboratory for Neurophysiology, https://sites.google.com/site/sohnlab2014/home Department of Biological SciencesKAIST
Dr. Hyun Yong Koh Translational Neurogenetics LabGraduate School of Medical Science and EngineeringKAIST
Dr. Jaeson Jang Ph.D.Visual System and Neural Network LaboratoryDepartment of Bio and Brain Engineering KAIST
Sang Hyeon Ju M.D.Laboratory for NeurophysiologyDepartment of Biological SciencesKAIST
2021.08.26 View 14982
A Mechanism Underlying Most Common Cause of Epileptic Seizures Revealed
An interdisciplinary study shows that neurons carrying somatic mutations in MTOR can lead to focal epileptogenesis via non-cell-autonomous hyperexcitability of nearby nonmutated neurons
During fetal development, cells should migrate to the outer edge of the brain to form critical connections for information transfer and regulation in the body. When even a few cells fail to move to the correct location, the neurons become disorganized and this results in focal cortical dysplasia. This condition is the most common cause of seizures that cannot be controlled with medication in children and the second most common cause in adults.
Now, an interdisciplinary team studying neurogenetics, neural networks, and neurophysiology at KAIST has revealed how dysfunctions in even a small percentage of cells can cause disorder across the entire brain. They published their results on June 28 in Annals of Neurology.
The work builds on a previous finding, also by a KAIST scientists, who found that focal cortical dysplasia was caused by mutations in the cells involved in mTOR, a pathway that regulates signaling between neurons in the brain.
“Only 1 to 2% of neurons carrying mutations in the mTOR signaling pathway that regulates cell signaling in the brain have been found to include seizures in animal models of focal cortical dysplasia,” said Professor Jong-Woo Sohn from the Department of Biological Sciences. “The main challenge of this study was to explain how nearby non-mutated neurons are hyperexcitable.”
Initially, the researchers hypothesized that the mutated cells affected the number of excitatory and inhibitory synapses in all neurons, mutated or not. These neural gates can trigger or halt activity, respectively, in other neurons. Seizures are a result of extreme activity, called hyperexcitability. If the mutated cells upend the balance and result in more excitatory cells, the researchers thought, it made sense that the cells would be more susceptible to hyperexcitability and, as a result, seizures.
“Contrary to our expectations, the synaptic input balance was not changed in either the mutated or non-mutated neurons,” said Professor Jeong Ho Lee from the Graduate School of Medical Science and Engineering. “We turned our attention to a protein overproduced by mutated neurons.”
The protein is adenosine kinase, which lowers the concentration of adenosine. This naturally occurring compound is an anticonvulsant and works to relax vessels. In mice engineered to have focal cortical dysplasia, the researchers injected adenosine to replace the levels lowered by the protein. It worked and the neurons became less excitable.
“We demonstrated that augmentation of adenosine signaling could attenuate the excitability of non-mutated neurons,” said Professor Se-Bum Paik from the Department of Bio and Brain Engineering.
The effect on the non-mutated neurons was the surprising part, according to Paik. “The seizure-triggering hyperexcitability originated not in the mutation-carrying neurons, but instead in the nearby non-mutated neurons,” he said.
The mutated neurons excreted more adenosine kinase, reducing the adenosine levels in the local environment of all the cells. With less adenosine, the non-mutated neurons became hyperexcitable, leading to seizures.
“While we need further investigate into the relationship between the concentration of adenosine and the increased excitation of nearby neurons, our results support the medical use of drugs to activate adenosine signaling as a possible treatment pathway for focal cortical dysplasia,” Professor Lee said.
The Suh Kyungbae Foundation, the Korea Health Technology Research and Development Project, the Ministry of Health & Welfare, and the National Research Foundation in Korea funded this work.
-Publication:Koh, H.Y., Jang, J., Ju, S.H., Kim, R., Cho, G.-B., Kim, D.S., Sohn, J.-W., Paik, S.-B. and Lee, J.H. (2021), ‘Non–Cell Autonomous Epileptogenesis in Focal Cortical Dysplasia’ Annals of Neurology, 90: 285 299. (https://doi.org/10.1002/ana.26149)
-ProfileProfessor Jeong Ho Lee Translational Neurogenetics Labhttps://tnl.kaist.ac.kr/ Graduate School of Medical Science and Engineering KAIST
Professor Se-Bum Paik Visual System and Neural Network Laboratory http://vs.kaist.ac.kr/ Department of Bio and Brain EngineeringKAIST
Professor Jong-Woo Sohn Laboratory for Neurophysiology, https://sites.google.com/site/sohnlab2014/home Department of Biological SciencesKAIST
Dr. Hyun Yong Koh Translational Neurogenetics LabGraduate School of Medical Science and EngineeringKAIST
Dr. Jaeson Jang Ph.D.Visual System and Neural Network LaboratoryDepartment of Bio and Brain Engineering KAIST
Sang Hyeon Ju M.D.Laboratory for NeurophysiologyDepartment of Biological SciencesKAIST
2021.08.26 View 14982 -
 Rare Mutations May Have Big Impact on Schizophrenia Pathology
- Somatic mutations found only in brain cells disrupt synaptic function. -
Schizophrenia is a neurodevelopmental disorder that disrupts brain activity, producing hallucinations, delusions, and other cognitive disturbances. Researchers have long searched for genetic influences in the disease, but genetic mutations have been identified in only a small fraction—fewer than a quarter—of sequenced patients. Now a study shows that “somatic” gene mutations in brain cells could account for some of the disease’s neuropathology.
The results of the study, led by Professor Jeong Ho Lee at the Graduate School of Medical Science and Engineering in collaboration with the Stanley Medical Research Institute in the US, appeared in Biological Psychiatry.
Traditional genetic mutations, called germline mutations, occur in sperm or egg cells and are passed on to offspring by their parents. Somatic mutations, in contrast, occur in an embryo after fertilization, and they can show up throughout the body or in isolated pockets of tissues, making them much harder to detect from blood or saliva samples, which are typically used for such sequencing studies.
Recently, more-advanced genetic sequencing techniques have allowed researchers to detect somatic mutations and studies have shown that even mutations present at very low levels can have functional consequences. A previous study hinted that brain somatic mutations were associated with schizophrenia, but it was not powerful enough to cement an association between brain somatic mutations and schizophrenia.
In the current study, the researchers used deep whole-exome sequencing to determine the genetic code of all exomes, the parts of genes that encode proteins. The scientists sequenced postmortem samples from brain, liver, spleen, or heart tissue of 27 people with schizophrenia and 31 control participants allowing them to compare the sequences in the two tissues. Using a powerful analytic technique, the team identified an average of 4.9 somatic single-nucleotide variants, or mutations, in brain samples from people with schizophrenia, and 5.6 somatic single-nucleotide variants in brain samples from control subjects.
Although there were no significant quantitative differences in somatic single-nucleotide variants between schizophrenia and control tissue samples, the researchers found that the mutations in schizophrenia patients were found in genes already associated with schizophrenia. Of the germline mutations that had previously been associated with schizophrenia, the genes affected encode proteins associated with synaptic neural communication, particularly in a brain region called the dorsolateral prefrontal cortex.
In the new analysis, the researchers determined which proteins might be affected by the newly identified somatic mutations. Remarkably, a protein called GRIN2B emerged as highly affected and two patients with schizophrenia carried somatic mutations on the GRIN2B gene itself. GRIN2B is a protein component of NMDA-type glutamate receptors, which are critical for neural signaling. Faulty glutamate receptors have long been suspected of contributing to schizophrenia pathology; GRIN2B ranks among the most-studied genes in schizophrenia. The somatic mutations identified in the study had a variant allele frequency of only ~1%, indicating that the mutations were rare among brain cells as a whole. Nevertheless, they have the potential to create widespread cortical dysfunction.
Professor Lee said, “Besides the comprehensive genetic analysis of brain-only mutations in postmortem tissues from schizophrenia patients, this study experimentally showed the biological consequence of identified somatic mutations, which led to neuronal abnormalities associated with schizophrenia. Thus, this study suggests that brain somatic mutations can be a hidden major contributor to schizophrenia and provides new insights into the molecular genetic architecture of schizophrenia.
John Krystal, MD, editor of Biological Psychiatry, said of the work, "The genetics of schizophrenia has received intensive study for several decades. Now a new possibility emerges, that in some cases, mutations in the DNA of brain cells contributes to the biology of schizophrenia. Remarkably this new biology points to an old schizophrenia story: NMDA glutamate receptor dysfunction. Perhaps the path through which somatic mutations contribute to schizophrenia converges with other sources of abnormalities in glutamate signaling in this disorder."
Professor Lee and the team next want to assess the functional consequences of the somatic mutations. Because of the location of the GRIN2B mutations found in schizophrenia patients, the researchers hypothesized that they might interfere with the receptors’ localization on neurons. Experiments on the cortical neurons of mice showed that the mutations indeed disrupted the receptors’ usual localization to dendrites, the “listening” ends of neurons, which in turn prevented the formation of normal synapses in the neurons. This finding suggests that the somatic mutations could disrupt neural communication, contributing to schizophrenia pathology.
- Profile:
Professor Jeong Ho Lee
Translational Neurogenetics Laboratory ( https://tnl.kaist.ac.kr/)
The Graduate School of Medical Science and Engineering
KAIST
(END)
2021.03.11 View 8842
Rare Mutations May Have Big Impact on Schizophrenia Pathology
- Somatic mutations found only in brain cells disrupt synaptic function. -
Schizophrenia is a neurodevelopmental disorder that disrupts brain activity, producing hallucinations, delusions, and other cognitive disturbances. Researchers have long searched for genetic influences in the disease, but genetic mutations have been identified in only a small fraction—fewer than a quarter—of sequenced patients. Now a study shows that “somatic” gene mutations in brain cells could account for some of the disease’s neuropathology.
The results of the study, led by Professor Jeong Ho Lee at the Graduate School of Medical Science and Engineering in collaboration with the Stanley Medical Research Institute in the US, appeared in Biological Psychiatry.
Traditional genetic mutations, called germline mutations, occur in sperm or egg cells and are passed on to offspring by their parents. Somatic mutations, in contrast, occur in an embryo after fertilization, and they can show up throughout the body or in isolated pockets of tissues, making them much harder to detect from blood or saliva samples, which are typically used for such sequencing studies.
Recently, more-advanced genetic sequencing techniques have allowed researchers to detect somatic mutations and studies have shown that even mutations present at very low levels can have functional consequences. A previous study hinted that brain somatic mutations were associated with schizophrenia, but it was not powerful enough to cement an association between brain somatic mutations and schizophrenia.
In the current study, the researchers used deep whole-exome sequencing to determine the genetic code of all exomes, the parts of genes that encode proteins. The scientists sequenced postmortem samples from brain, liver, spleen, or heart tissue of 27 people with schizophrenia and 31 control participants allowing them to compare the sequences in the two tissues. Using a powerful analytic technique, the team identified an average of 4.9 somatic single-nucleotide variants, or mutations, in brain samples from people with schizophrenia, and 5.6 somatic single-nucleotide variants in brain samples from control subjects.
Although there were no significant quantitative differences in somatic single-nucleotide variants between schizophrenia and control tissue samples, the researchers found that the mutations in schizophrenia patients were found in genes already associated with schizophrenia. Of the germline mutations that had previously been associated with schizophrenia, the genes affected encode proteins associated with synaptic neural communication, particularly in a brain region called the dorsolateral prefrontal cortex.
In the new analysis, the researchers determined which proteins might be affected by the newly identified somatic mutations. Remarkably, a protein called GRIN2B emerged as highly affected and two patients with schizophrenia carried somatic mutations on the GRIN2B gene itself. GRIN2B is a protein component of NMDA-type glutamate receptors, which are critical for neural signaling. Faulty glutamate receptors have long been suspected of contributing to schizophrenia pathology; GRIN2B ranks among the most-studied genes in schizophrenia. The somatic mutations identified in the study had a variant allele frequency of only ~1%, indicating that the mutations were rare among brain cells as a whole. Nevertheless, they have the potential to create widespread cortical dysfunction.
Professor Lee said, “Besides the comprehensive genetic analysis of brain-only mutations in postmortem tissues from schizophrenia patients, this study experimentally showed the biological consequence of identified somatic mutations, which led to neuronal abnormalities associated with schizophrenia. Thus, this study suggests that brain somatic mutations can be a hidden major contributor to schizophrenia and provides new insights into the molecular genetic architecture of schizophrenia.
John Krystal, MD, editor of Biological Psychiatry, said of the work, "The genetics of schizophrenia has received intensive study for several decades. Now a new possibility emerges, that in some cases, mutations in the DNA of brain cells contributes to the biology of schizophrenia. Remarkably this new biology points to an old schizophrenia story: NMDA glutamate receptor dysfunction. Perhaps the path through which somatic mutations contribute to schizophrenia converges with other sources of abnormalities in glutamate signaling in this disorder."
Professor Lee and the team next want to assess the functional consequences of the somatic mutations. Because of the location of the GRIN2B mutations found in schizophrenia patients, the researchers hypothesized that they might interfere with the receptors’ localization on neurons. Experiments on the cortical neurons of mice showed that the mutations indeed disrupted the receptors’ usual localization to dendrites, the “listening” ends of neurons, which in turn prevented the formation of normal synapses in the neurons. This finding suggests that the somatic mutations could disrupt neural communication, contributing to schizophrenia pathology.
- Profile:
Professor Jeong Ho Lee
Translational Neurogenetics Laboratory ( https://tnl.kaist.ac.kr/)
The Graduate School of Medical Science and Engineering
KAIST
(END)
2021.03.11 View 8842 -
 Life After COVID-19: Big Questions on Medical and Bio-Engineering
KAIST GSI forum explores big questions in the medical and bio-engineering revolution caused by the COVID-19 in fight against infectious diseases and life quality
On September 9, the Global Strategy Institute at KAIST will delve into innovative future strategies for the medical and bio-engineering sectors that have been disrupted by COVID-19. The forum will live stream via YouTube, KTV, and Naver TV from 9:00 am Korean time.
The online forum features a speaker lineup of world-renowned scholars who will discuss an array of bio-engineering technologies that will improve our quality of life and even extend our life span. This is the GSI’s third online forum since the first one in April that covered the socio-economic implications of the global pandemic and the second one in June focusing on the education sector.
In hosting the third round of the GSI Forum series, KAIST President Sung-Chul Shin stressed the power of science and technology saying, “In this world full of uncertainties, one thing for sure is that only the advancement of science and technology will deliver us from this crisis.” Korean Prime Minister Sye-Kyun Chung will also deliver a speech explaining the government’s response to COVID-19 and vaccine development strategies.
The President of the National Academy of Medicine in the US will share ideal policies to back up the bio-engineering and medical sectors and Futurist Thomas Frey from the Davinci Institute will present his distinct perspectives on our future lives after COVID-19. His thought-provoking insights on advancements in the bioengineering sector will examine whether humanity can put an end to infectious diseases and find new ways to lengthen our lives.
Two distinguished professors in the field of genetic engineering technology will share their latest breakthroughs. Professor George McDonald Church from Harvard Medical School who developed genome sequencing will deliver a keynote speech on how the advancement of gene editing and genome technology will overcome diseases and contribute to extending human life spans.
Professor Kwang-Soo Kim, a KAIST alumnus from Harvard Medical School who recently reported new discoveries for Parkinson’s disease treatment by reprogramming a patient’s own skin cells to replace cells in the brain, will introduce the latest clinical cell treatment technologies based on personalized therapeutics.
Senior Vice President and Chief Product Officer of Illumina Susan Tousi, a leading genome sequencing solution provider, will describe genome analysis technology and explore the potential for disease prevention.
KAIST medical scientist Jeong Ho Lee, who was the first to identify the causes of intractable epilepsies and has identified the genes responsible for several developmental brain disorders. Professor Jin-Hyung Lee from Stanford University and Dr. David B. Resnik from the National Institute of Environmental Health Science will also join the speaker lineup to discuss genetics-based personalized solutions to extend human life spans.
The forum will also invite about 50 young scientists and medical researchers from around the world to participate in an online panel session. They will engage in a Q&A session and a discussion with the speakers.
(END)
2020.09.04 View 11753
Life After COVID-19: Big Questions on Medical and Bio-Engineering
KAIST GSI forum explores big questions in the medical and bio-engineering revolution caused by the COVID-19 in fight against infectious diseases and life quality
On September 9, the Global Strategy Institute at KAIST will delve into innovative future strategies for the medical and bio-engineering sectors that have been disrupted by COVID-19. The forum will live stream via YouTube, KTV, and Naver TV from 9:00 am Korean time.
The online forum features a speaker lineup of world-renowned scholars who will discuss an array of bio-engineering technologies that will improve our quality of life and even extend our life span. This is the GSI’s third online forum since the first one in April that covered the socio-economic implications of the global pandemic and the second one in June focusing on the education sector.
In hosting the third round of the GSI Forum series, KAIST President Sung-Chul Shin stressed the power of science and technology saying, “In this world full of uncertainties, one thing for sure is that only the advancement of science and technology will deliver us from this crisis.” Korean Prime Minister Sye-Kyun Chung will also deliver a speech explaining the government’s response to COVID-19 and vaccine development strategies.
The President of the National Academy of Medicine in the US will share ideal policies to back up the bio-engineering and medical sectors and Futurist Thomas Frey from the Davinci Institute will present his distinct perspectives on our future lives after COVID-19. His thought-provoking insights on advancements in the bioengineering sector will examine whether humanity can put an end to infectious diseases and find new ways to lengthen our lives.
Two distinguished professors in the field of genetic engineering technology will share their latest breakthroughs. Professor George McDonald Church from Harvard Medical School who developed genome sequencing will deliver a keynote speech on how the advancement of gene editing and genome technology will overcome diseases and contribute to extending human life spans.
Professor Kwang-Soo Kim, a KAIST alumnus from Harvard Medical School who recently reported new discoveries for Parkinson’s disease treatment by reprogramming a patient’s own skin cells to replace cells in the brain, will introduce the latest clinical cell treatment technologies based on personalized therapeutics.
Senior Vice President and Chief Product Officer of Illumina Susan Tousi, a leading genome sequencing solution provider, will describe genome analysis technology and explore the potential for disease prevention.
KAIST medical scientist Jeong Ho Lee, who was the first to identify the causes of intractable epilepsies and has identified the genes responsible for several developmental brain disorders. Professor Jin-Hyung Lee from Stanford University and Dr. David B. Resnik from the National Institute of Environmental Health Science will also join the speaker lineup to discuss genetics-based personalized solutions to extend human life spans.
The forum will also invite about 50 young scientists and medical researchers from around the world to participate in an online panel session. They will engage in a Q&A session and a discussion with the speakers.
(END)
2020.09.04 View 11753 -
 Professor J.H. Lee Wins the Innovators in Science Award
Professor Jeong Ho Lee from the Graduate School of Medical Science and Engineering won the Early-Career Scientist Award of the 2020 Innovators in Science Award. The New York Academy of Sciences administers the award in partnership with Takeda Pharmaceutical Company.
The Innovators in Science Award grants two prizes of US $200,000 each year: one to an Early-Career Scientist and the other to a well-established Senior Scientist who have distinguished themselves for the creative thinking and impact of their rare disease research. The Senior Scientist Awardee is Dr. Adrian R. Krainer, at Cold Spring Harbor Laboratory whose research focused on the mechanisms and control of RNA splicing.
Prof. Lee is recognized for his research investigating genetic mutations in stem cells in the brain that result in rare developmental brain disorders. He was the first to identify the causes of intractable epilepsies and has identified the genes responsible for several developmental brain disorders, including focal cortical dysplasia, Joubert syndrome—a disorder characterized by an underdevelopment of the brainstem—and hemimegaloencephaly, which is the abnormal enlargement of one side of the brain.
“It is a great honor to be recognized by a jury of such globally respected scientists whom I greatly admire,” said Prof. Lee. “More importantly, this award validates research into brain somatic mutations as an important area of exploration to help patients suffering from devastating and untreatable neurological disorders.”
Prof. Lee also is the Director of the National Creative Research Initiative Center for Brain Somatic Mutations, and Co-founder and Chief Technology Officer of SoVarGen, a biopharmaceutical company aiming to discover novel therapeutics and diagnosis for intractable central nervous system (CNS) diseases caused by low-level somatic mutation.
The Innovators in Science Award is a limited submission competition in which research universities, academic institutions, government or non-profit institutions, or equivalent from around the globe with a well-established record of scientific excellence are invited to nominate their most promising Early-Career Scientists and their most outstanding Senior Scientists working in one of four selected therapeutic fields of neuroscience, gastroenterology, oncology, and regenerative medicine. The 2020 Winners will be honored at the virtual Innovators in Science Award Ceremony and Symposium in October 2020.
2020.07.09 View 11177
Professor J.H. Lee Wins the Innovators in Science Award
Professor Jeong Ho Lee from the Graduate School of Medical Science and Engineering won the Early-Career Scientist Award of the 2020 Innovators in Science Award. The New York Academy of Sciences administers the award in partnership with Takeda Pharmaceutical Company.
The Innovators in Science Award grants two prizes of US $200,000 each year: one to an Early-Career Scientist and the other to a well-established Senior Scientist who have distinguished themselves for the creative thinking and impact of their rare disease research. The Senior Scientist Awardee is Dr. Adrian R. Krainer, at Cold Spring Harbor Laboratory whose research focused on the mechanisms and control of RNA splicing.
Prof. Lee is recognized for his research investigating genetic mutations in stem cells in the brain that result in rare developmental brain disorders. He was the first to identify the causes of intractable epilepsies and has identified the genes responsible for several developmental brain disorders, including focal cortical dysplasia, Joubert syndrome—a disorder characterized by an underdevelopment of the brainstem—and hemimegaloencephaly, which is the abnormal enlargement of one side of the brain.
“It is a great honor to be recognized by a jury of such globally respected scientists whom I greatly admire,” said Prof. Lee. “More importantly, this award validates research into brain somatic mutations as an important area of exploration to help patients suffering from devastating and untreatable neurological disorders.”
Prof. Lee also is the Director of the National Creative Research Initiative Center for Brain Somatic Mutations, and Co-founder and Chief Technology Officer of SoVarGen, a biopharmaceutical company aiming to discover novel therapeutics and diagnosis for intractable central nervous system (CNS) diseases caused by low-level somatic mutation.
The Innovators in Science Award is a limited submission competition in which research universities, academic institutions, government or non-profit institutions, or equivalent from around the globe with a well-established record of scientific excellence are invited to nominate their most promising Early-Career Scientists and their most outstanding Senior Scientists working in one of four selected therapeutic fields of neuroscience, gastroenterology, oncology, and regenerative medicine. The 2020 Winners will be honored at the virtual Innovators in Science Award Ceremony and Symposium in October 2020.
2020.07.09 View 11177 -
 Professor Jeong Ho Lee Receives the 2015 Pediatric Epilepsies Research Award
The award identifies leading scientists worldwide and funds their cutting-edge research in epilepsy.
The Citizen United for Research in Epilepsy (CURE) announced on September 7, 2015, that Jeong Ho Lee, a professor of the Graduate School of Medical Science and Engineering at KAIST, will be awarded the 2015 Pediatric Epilepsies Research Award.
The Pediatric Epilepsies Research Award is given annually to a researcher who has conducted novel, innovative research projects that address severe, intractable pediatric epilepsies as well as collaborative, interdisciplinary projects that explore new approaches to find a treatment for pediatric epilepsies.
Lee was recognized for his leading study in the field of intractable epilepsy. He is the first Korean who has ever received this award, securing a research grant of USD 250,000 for two years.
Lee has conducted research on brain somatic mutations as the novel cause of childhood intractable epilepsy. Pediatric epilepsies account for approximately 70% of all cases of epilepsy.
Established in 1998, CURE is a non-profit American organization based in Chicago, Illinois, which is committed to funding research and various initiatives that will lead to breakthroughs to cure epilepsy.
Since its inception, CURE has been at the forefront of epilepsy research, raising more than USD 32 million to support researchers and scientists worldwide. It has also awarded more than 180 cutting-edge projects in 13 countries.
2015.09.09 View 11941
Professor Jeong Ho Lee Receives the 2015 Pediatric Epilepsies Research Award
The award identifies leading scientists worldwide and funds their cutting-edge research in epilepsy.
The Citizen United for Research in Epilepsy (CURE) announced on September 7, 2015, that Jeong Ho Lee, a professor of the Graduate School of Medical Science and Engineering at KAIST, will be awarded the 2015 Pediatric Epilepsies Research Award.
The Pediatric Epilepsies Research Award is given annually to a researcher who has conducted novel, innovative research projects that address severe, intractable pediatric epilepsies as well as collaborative, interdisciplinary projects that explore new approaches to find a treatment for pediatric epilepsies.
Lee was recognized for his leading study in the field of intractable epilepsy. He is the first Korean who has ever received this award, securing a research grant of USD 250,000 for two years.
Lee has conducted research on brain somatic mutations as the novel cause of childhood intractable epilepsy. Pediatric epilepsies account for approximately 70% of all cases of epilepsy.
Established in 1998, CURE is a non-profit American organization based in Chicago, Illinois, which is committed to funding research and various initiatives that will lead to breakthroughs to cure epilepsy.
Since its inception, CURE has been at the forefront of epilepsy research, raising more than USD 32 million to support researchers and scientists worldwide. It has also awarded more than 180 cutting-edge projects in 13 countries.
2015.09.09 View 11941